Nestlé Health Science UK Statement on Demand for Specialist Infant Formulas for Cows’ Milk and Multiple Food Allergies
We believe breast milk is the best food for infants. When in consultation with their healthcare professional, mothers and families find that optimal breastfeeding is not possible due to their infant’s medical condition, formulas for special medical purposes play a vital role in providing essential nutrients to infants. We have a global commitment to market breast-milk substitutes responsibly.
This website is about the management of cows’ milk protein allergy and nutritional solutions intended for infants. By continuing on this website, you accept that Nestlé Health Science supplies the information at your own request.
Are you a healthcare professional (HCP) or a parent?
Cows’ milk allergy (CMA) also known as cows’ milk protein allergy (CMPA) often presents with diverse and non-specific symptoms, making it challenging to diagnose and manage.1 At Nestlé Health Science, we understand this challenge and are committed to supporting healthcare professionals, patients and caregivers in caring for infants with CMA.
KEY FACTS ABOUT COWS' MILK PROTEIN ALLERGY
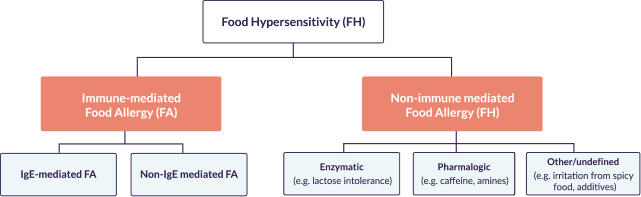
Cows' milk allergy (CMA) is one of the most common food allergies in the first year of life. It occurs when an infant’s immune system reacts abnormally to the proteins in cows' milk, which are either transferred from the mother while breastfeeding or from cows' milk protein-containing formulas and complementary food. The immune reaction may be immunoglobulin (Ig)E-mediated, non-IgE-mediated, or mixed. The reactions can be immediate (early) reactions, occurring from minutes to hours after exposure, and/or delayed (late) reactions, which can manifest 48 hours or even a week following ingestion. Immediate reactions are more likely to involve IgE, but combinations of immediate and delayed reactions can occur in some infants.1
IgE mediated food allergies
- Immediate reaction: onset of symptoms within minutes or up to 2 hours after ingesting the suspected food
- Can be severe, i.e. anaphylaxis or non-severe, i.e. rash
- IgE antibodies cause the release of cytokines and hystamines which trigger an inflammatory response
Non-IgE mediated food allergies
- Delayed reaction: onset of symptoms within hours or days after ingesting the suspected food
- Mediated by the T cells of the immune system, which trigger IgG and IgA antibodies
- Mechanism still poorly defined
- Prevalence in the UK of up to 56% of CMA cases being Non-IgE
Prospective cohort studies in Europe suggest a 10-year prevalence of 1.9% to 4.9% for CMA in infancy.3 A UK prospective birth cohort study reflect this with an incidence rate of 2.3% in 1-3 year olds.4
Prognosis of non-IgE and IgE food allergy varies in the literature. The large EuroPrevall prospective birth cohort study showed 100% of children with non-IgE mediated allergy were tolerant at 1 after diagnosis, with 56.5% of children with IgE becoming tolerant at 1 year after diagnosis.5
Non-allergic food hypersensitivities, such as intolerances, result from the inability to digest certain components of foods, i.e. lactose or fructose, or, less commonly, food coloring, additives or preservatives. Non-allergic food hypersensitivities do not involve the immune system and are much more common than food allergies.1
Food allergies arise through an immunological reaction to certain allergens in food. These allergens are usually proteins.6 Other components in food, such as lactose and other carbohydrates, do not commonly act as allergens.
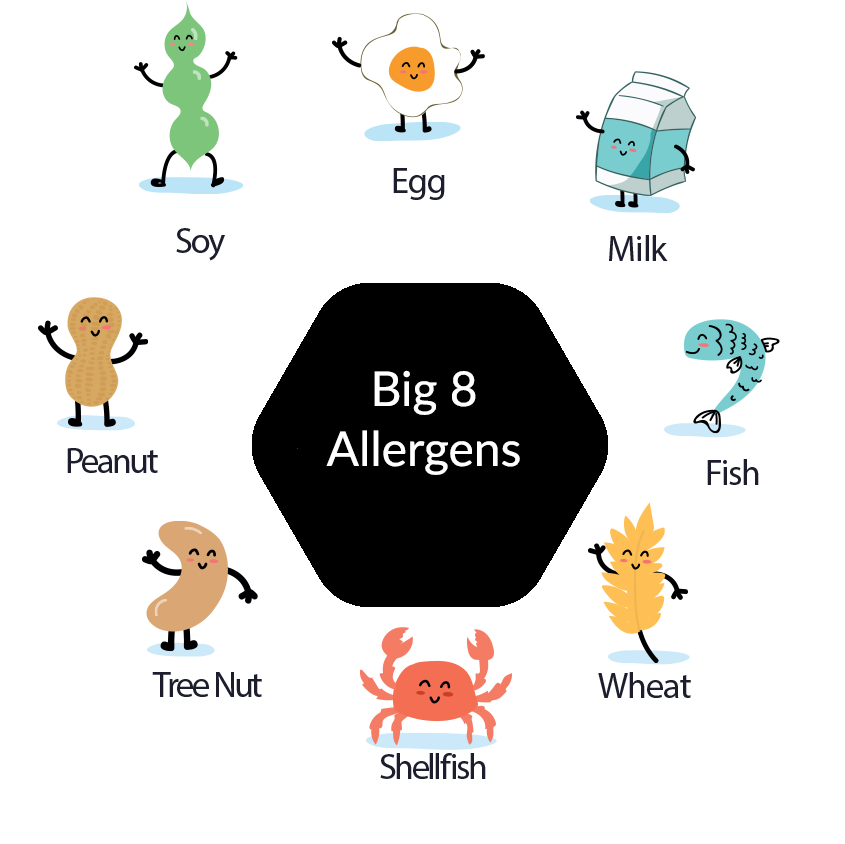
Certain allergens cause more reactions than others. In no particular order, here are the eight most common allergens accounting for approximately 90 percent of all allergic reactions to food in children.7
Food allergy is an increasing health concern in infants and young children.1
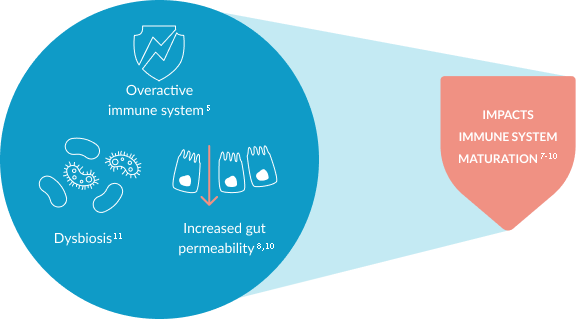
CMA is an immune-mediated disease. It is associated with an overactive immune system, increased gut permeability and dysbiosis, which might affect the maturation of an infants’ immune system.6-12 This can lead to an increased risk of infections and future allergies.13-15
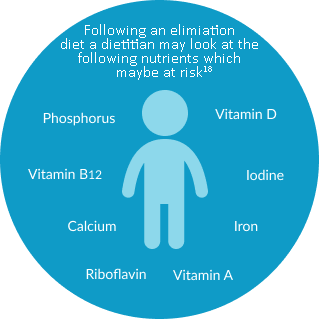
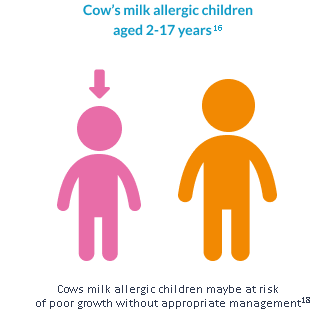
When following an elimination diet without dietetic support, breastfed children with CMA and/or multiple food allergies are at an increased risk of nutritional deficiencies,16 which can lead to significantly lower growth parameters.17 As infants with food allergies start complementary feeding, continued dietetic support is therefore important, as it can be challenging for caregivers to provide an appropriate elimination diet which ensures a sufficient energy and nutrient intake.18
Lactose is a disaccharide comprising of glucose and galactose.20 As a key component of breast milk, lactose is important for healthy growth and development, providing energy and supporting the absorption of calcium.21 Lactose inhibits putrefactive bacteria and promotes the development of healthy gut microbiota.22 Therefore, it is not recommended that lactose is eliminated from the infant’s diet.
In specialist infant formulas for babies not on breast milk, lactose also has another important benefit: it improves their taste. The pleasant taste and aroma of lactose contribute toward improved acceptance of extensively hydrolysed formulas (eHFs) intended for the management of CMA in formula fed-infants.23 This reinforces the importance of lactose in the infant’s diet.
Lactose intolerance results from a decreased ability to digest and absorb lactose (the sugar present in mammalian milk) due to a lack of the enzyme lactase. It is very rare in infants and children younger than 5 years,21 even in those with CMA.
Breast milk naturally contains a high amount of lactose, which is beneficial for healthy infant growth and development.22
| CMA Prevelance | Lactose Intolerance Prevelance |
|---|---|
| 2.3% of infants ≤1 year24> | As a key component of human breastmilk, it is very rare in children ≤5 years21 65% of people globally have lactose intolerance in adulthood23 |
NESTLÉ HEALTH SCIENCE: SUPPORTING COWS' MILK ALLERGY DIAGNOSIS AND MANAGEMENT
CMA can be a challenge to diagnose given the large variability in number and severity of the symptoms, and the fact that some of them are perfectly normal for infants to experience.
At Nestlé Health Science, we understand this challenge and are committed to providing leading expert-developed tools, nutritional solutions and support for healthcare professionals to help facilitate the earlier diagnosis and appropriate management of infants and young children with CMA. We are also dedicated to providing information, tools and support for caregivers to help raise awareness around the symptoms of CMA

SIGNS AND SYMPTOMS
Inconsolable crying, colic, skin rashes, vomiting, diarrhoea, and constipation are all common signs and symptoms of CMA, especially in early infancy.
SIGNS & SYMPTOMS
CONSIDER CMA
Leading experts have developed the Cows' Milk-related Symptom Score (CoMiSSTM) to help healthcare professionals recognise and assess non-specific signs and symptoms that could be indicative of CMA.
COMISS® TOOL
CLARIFY THE DIAGNOSIS
Diagnosing CMA can often be challenging, and tests are available to help assess the presence of IgE CMA. In non-IgE CMA, the quality standard for diagnosing it is the elimination diet, which is a diet free from cows' milk protein, followed by a food challenge.25
DIAGNOSING CMAOUR RANGE OF TAILOR-MADE NUTRITIONAL SOLUTIONS FOR FORMULA FED BABIES
The Nestlé Health Science range of hypoallergenic nutritional solutions, SMA Althéra and SMA Alfamino, are tailor-made to help meet the specific nutritional needs of non-breastfed infants with CMA.
NESTLÉ’S HEALTH SCIENCE’S COMMITMENT TO CMA EDUCATION & RESOURCES
Nestlé Health Science is dedicated to developing and sharing leading scientific information and educational tools and resources to support in the identification and management of CMA for healthcare professionals and to help caregivers during their journey with CMA

EXPERT CORNER:
CMA DIAGNOSIS
Leading experts in paediatric gastroenterology and food allergy answer common questions related to the diagnosis of CMA in our online video series.
WATCH NOW
CASE STUDIES
Understand some of the diagnostic and management challenges – from the initial symptom presentation to diagnosis followed by the dietary management in a series of case studies.
READ MORE
SUPPORT FOR PARENTS AND CAREGIVERS
Information and tools are available for parents to support them along their CMA journey.
FIND MATERIALS- Koletzko S, et al. Diagnostic Approach and Management of Cows'-Milk Protein Allergy in Infants and Children: ESPGHAN Gl Committee Practical Guidelines. JPGN 2012;55:221–9
- NICE CKS. Cows' milk allergy in children. NICE. 2019. Cows' milk allergy in children | Health topics A to Z | CKS | NICE
- Venter C et al. Diagnosis and management of non-IgE-mediated cows' milk allergy in infancy – a UK primary care practical guide. Clinical and Translational Allergy. 2013;3(1):23
- Venter, C., Pereira, B., Voigt, K. et al. (2008) Prevalence and cumulative incidence of food hypersensitivity in the first 3 years of life. Allergy 63(3), 354-359.
- Schoemaker, A.A., Sprikkelman, A.B., Grimshaw, K.E. et al. (2015) Incidence and natural history of challenge-proven cows' milk allergy in European children - EuroPrevall birth cohort. Allergy 70(8), 963-972.
- NHS Choices. Food Allergy.2016 Available at: https://www.nhs.uk/conditions/food-allergy/ (Accessed April 2021).
- US FDA. Food Allergies: What You Need to Know. Available at: https://www.fda.gov/food/buy-store-serve-safe-food/what-you-need-know-about-food-allergies (accessed August 2020).
- Jalonen T. Identical intestinal permeability changes in children with different clinical manifestations of cows' milk allergy. J allergy Clin Immunol 1991;88(5):737-742.
- Crittenden RG and Bennett LE. Cows' Milk Allergy: A Complex Disorder. J Am Coll Nutr 2005;24(6suppl):582S–591S.
- Thompson-Chagoyan OC, et al. Faecal Microbiota and Short-Chain Fatty Acid Levels in Faeces from Infants with Cows' Milk Protein Allergy. Int Arch Allergy Immunol 2011;156(3):325–332.
- Azad MB, et al. Infant gut microbiota and food sensitization: associations in the first year of life. Clin Exp Allergy 2015;45(3):632-643.
- Chin AM, et al. Morphogenesis and maturation of the embryonic and postnatal intestine. Semin Cell Dev Biol 2017;66:81-93.
- Tanaka M and Nakayama J. Development of the gut microbiota in infancy and its impact on health in later life. Allergol Int 2017;66(4):515-522.
- Dzidic M, et al. Gut Microbiota and Mucosal Immunity in the Neonate. Med Sci (Basel). 2018;6(3):56.
- Juntti H, et al. Cows' Milk Allergy is Associated with Recurrent Otitis Media During Childhood. Acta Otolaryngol 1999;119(8):867-873.
- Tikkanen S, et al. Status of children with cows' milk allergy in infancy by 10 years of Age. Acta Paediatr 2000; 89(10):1174-1180.
- Woicka-Kolejwa K, et al. Food allergy is associated with recurrent respiratory tract infections during childhood. Postepy Dermatol Alergol 2016;33(2):109-113.
- ASCIA 2017 – Food Allergy Clinical Update for Dietitians. Received from https://etrainingdiet.ascia.org.au/login/index.php on 5th June 2019.
- Nwaru BI, et al., on behalf of the EAACI Food Allergy and Anaphylaxis Guidelines Group. Prevalence of common food allergies in Europe: A systematic review and meta-analysis. Allergy 2014; 69 :992-1007
- Robbins et al. Milk allergy is associated with decreased growth in U.S. children. J Allergy Clin Immunol. 2014 December; 134(6):1466-1468.
- Meyer, R. Nutritional disorders resulting from food allergy in children. Pediatr Allergy Immunol. 2018; 29:689– 704. https://doi.org/10.1111/pai.12960
- Heyman MB et al. Committee on Nutrition. Lactose intolerance in infants, children, and adolescents. Pediatrics. 2006;118(3):1279–86.
- Abrams S. et al. Calcium and zinc absorption from lactose-containing and lactose free infant formulas. Am J Clin Nutr, 2002; 76:442–6.
- Francavilla R et al. Effect of lactose on gut microbiota and metabolome of infants with cows' milk allergy. Pediatr Allergy Immunol. 2012;23(5):420–7.
- Luyt D et al. BSACI Milk allergy guideline. Clinical & Experimental Allergy, 2014 (44) 642–672.
- NICE. Food Allergy NICE (QS118). 2016.
IMPORTANT NOTICE: Mothers should be encouraged to continue breastfeeding even when their babies have cows' milk protein allergy. This usually requires qualified dietary counselling to completely exclude all sources of cows' milk protein from the mothers’ diet. If a decision to use a special formula intended for infants is taken, it is important to follow the instructions on the label. Unboiled water, unboiled bottles or incorrect dilution can make babies ill. Incorrect storage, handling, preparation and feeding can eventually lead to adverse effects on the health of babies. Formula for special medical purposes intended for infants must be used under medical supervision.